Opioids have been used to relieve pain for thousands of years but the past three decades have seen an explosion in their medical and non-medical use.
The harms caused by opioids — including dependence, overdose and death — are an international public health concern.
In particular, the devastating impact of opioids in North America is increasingly coming to light in multi-billion-dollar civil settlements, a Netflix series and widespread media coverage.
Australia also saw opioid use grow to one of the highest in the world, with opioid deaths increasing by 62% between 2001 and 2016.
This led to a range of strategies implemented in recent years to address the problems of opioid use.
But have these measures worked, and should Australia still be concerned about an opioid epidemic on the scale of North America’s? Here’s what you need to know about opioids in Australia.
What are opioids?
Opioids are a group of drugs that relax the body and can relieve pain. They can be derived from the poppy plant or be man-made. They work by attaching to opioid receptors on nerve cells, blocking pain messages sent by the body.
Common types of opioid-based medications include codeine (which is found in Panadeine, Panadeine Forte and Nurofen Plus), fentanyl, morphine, oxycodone (Endone or OxyContin), buprenorphine (Subutex or Suboxone), methadone and tramadol.
Heroin is an opioid used non-medically for its euphoric effects, but all opioid medications may be used for this reason.
Although opioids can be effective in helping manage pain, they may not provide long-term improvements in pain or function, compared with placebo or non-opioid medications.
Their non-medical use, prolonged use, misuse and use without medical supervision can lead to opioid dependence, a range of other health problems and death.
North America’s opioid epidemic
The opioid epidemic is one of the worst public health disasters affecting the USA and Canada.
It’s estimated that nearly 600,000 Americans died of opioid-involved overdoses in the past two decades, with an estimated 1.2 million more deaths expected by 2029.
The crisis has been driven by several factors; most significantly, changes to how pharmaceutical opioids were prescribed.
These drugs were initially used to treat pain that was short-term, terminal or related to cancer but in the 1990s, pharmaceutical companies began marketing opioids for chronic pain, despite limited evidence of efficacy or safety in many of those patients.
“We did see a large increase in the use of prescription opioids, a lot of promotion of prescription opioids, and also promotion that they were safe and they were not likely to cause addiction or dependence, which we know now is categorically untrue,”
– Professor Suzanne Nielsen, the Deputy Director of the Monash Addiction Research Centre.
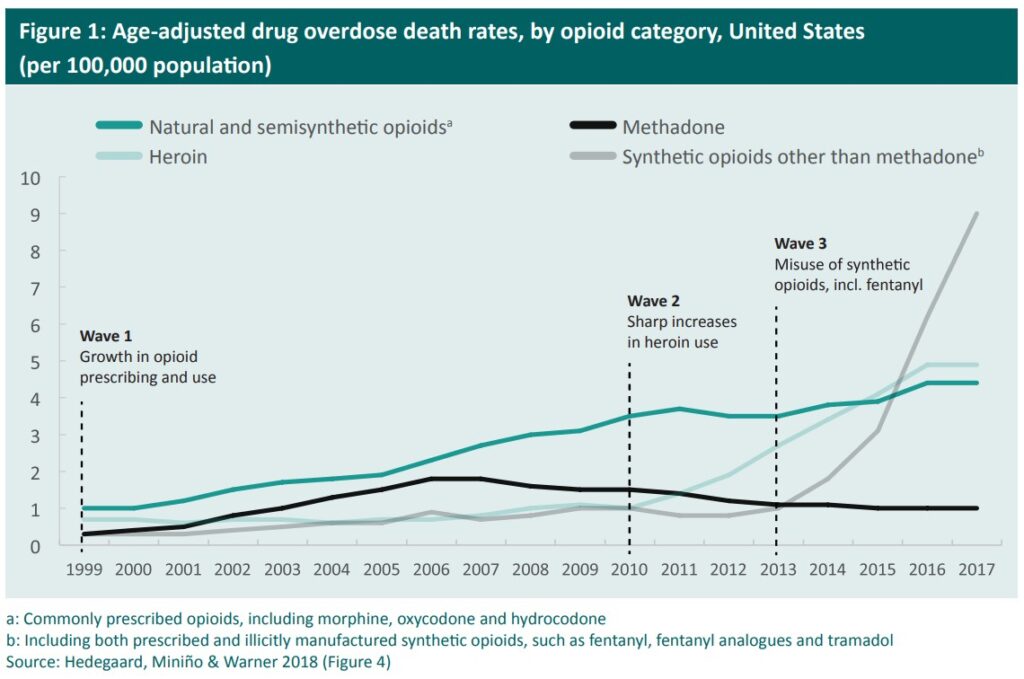
Liberal use of prescription opioids for pain relief kicked off three distinct but interconnected waves in the opioid epidemic in North America. The first was in the 1990s with a rise in overdose deaths involving prescription opioids.
The second was a sharp uptick in 2010, driven by new restrictive opioid prescription guidelines, making them harder to obtain, and reformulation of these drugs to reduce their effects. This meant many opioid-dependent people began using, and overdosing on, heroin.
The third wave in 2013 involved an increase in availability of synthetic opioids, especially fentanyl, which is approximately 50 times more potent than heroin.
Fentanyl targeted the heroin market as a powerful alternative or, more commonly, additive to heroin. It’s often mixed with other drugs like cocaine, with or without the users’ knowledge.
Overdose deaths are also the result of fake pharmaceutical opioids — that look like oxycodone pills — that are illicitly manufactured and often contain fentanyl.
Opioids in Australia
Since the early 1990s, Australia has seen a steady increase in the prescription of opioids to manage chronic pain.
From 2002 to 2019, the rate of drug overdose deaths involving opioids more than doubled (2.5 versus 5.0 deaths per 100,000 people, respectively), increasing on average by 5.1% per year and peaking at 5.8 deaths per 100,000 people in 2017.
In response, Australia introduced several measures to address opioid dependence and overdose, including stricter prescription conditions, rescheduling codeine (it’s now prescription-only instead of accessible over the counter), introducing prescription drug monitoring programs, abuse-deterrent formulations such as tamper-resistant tablets and smaller pack sizes, making take-home naloxone (a drug that can reverse opioid overdose) available over the counter for free, and improved access to Opioid Substitution Therapy (OST).
“We do have evidence that pharmaceutical opioid-related deaths are going down, but we also have some evidence that we’ve seen with these restrictions, some people potentially have shifted to illicit opioids and we’re seeing those deaths go up,”.
“So, it’s a complex picture.”– Professor Nielsen
Opioids are the most common cause of unintentional overdose deaths, and these are largely preventable. In 2021, there were 1,008 drug overdose deaths involving opioids among Australians.
These deaths typically occurred among males (64%, 642 deaths) and in the 45-54 (28%, 282 deaths) and 35-44 (27%, 268 deaths) age groups. Three in four (76%, 763 deaths) were considered unintentional.
“We have naloxone now available for free for all Australians through a commonwealth-funded program across the country, and you can get that without a prescription,”
“That’s one of the things Australia’s been on the front foot about, but we can do a lot more work to promote that.”– Professor Nielsen
Treatment for opioid dependence is becoming more accessible and affordable.
“Those are the substitution medications that people who are dependent on opioids can access, so methadone and buprenorphine, and the new long-acting injectable, which is a really positive step,”
“It’s now a lot more affordable for people, cost was a huge barrier, so instead of being quite onerous for people who needed to access that program, it’s just like another medicine now through the PBS.”– Robert Taylor, the Alcohol and Drug Foundation’s Knowledge Manager.
Overall, Australia’s approach is more health-oriented than law enforcement-focused.
“I’m optimistic that this stronger health focus will lead to better outcomes,”
“While it looks like the situation in Australia is not as dire as that in the US, we also have some warning signs that we need to be careful, and we need to make sure that we put things in place to try and prevent some of those large scale shifts to illicit opioids that really opened up the door for much more significant harms with this very toxic drug market.”– Professor Nielsen
The future of fentanyl
Fentanyl entering Australia is still a very real concern. In the United States, synthetic opioids like fentanyl accounted for 67,325 preventable deaths in 2021 – a 26% increase from the previous year.
And in Canada, deaths doubled in 2022 compared to before the COVID-19 pandemic.
“Nothing is impossible and it is a really, really serious fear in the drug and alcohol sector that we could end up with that situation,”
– Taylor
Mexico and China are the primary sources for fentanyl and fentanyl-related substances trafficked into North America. The presence of fentanyl has not been widely identified in Australia’s illicit drug market.
“There’ve been studies that have tried to estimate what would happen if we did suddenly have an introduction of fentanyl into our supply and the modelling suggested that the overdose death toll would go up four or five times, which would be terrible,”
– Taylor
Authorities have intercepted an increasing number of shipments of illicit fentanyl heading to Australia.
In late 2022, the Australian Federal Police seized the largest shipment ever detected in Australia, containing more than five million potentially lethal doses of the drug.
“Law enforcement do their best to block the supply of those things coming into the country, but the reality is — we know drugs come into the country every day, and [law enforcement] is not going to be enough,”
– Taylor
A harm-reduction approach to opioid dependence is required to limit injury or death from drug use, with strategies to support the individual to seek treatment at some stage.
These include needle and syringe programs for safe injecting and disposal of equipment, overdose prevention sites or safe injecting rooms where teams of trained staff monitor people who use illicit drugs, and access to opioid substitution therapy.
“A lot of risk for drug and alcohol harm comes down to risk factors in someone’s life,”
“Poor mental health, challenges with housing, challenges in relationships, economic insecurity, unemployment — all these risk factors contribute to the likelihood of someone experiencing harmful drug use. So if we have a healthy community, there’s much more resilience and there’s less risk that those harms do occur.”– Taylor
If you want more information about opioids or you’re worried about your own, or someone else’s use, call the the Alcohol and Other Drug Hotline on 1800 250 015.












