It seems obvious but looking after your heart is vital to your long-term health.
If you don’t, the results can be devastating — cardiovascular disease (a term used to refer to a group of disorders that affect the heart and blood vessels) is the leading cause of illness and death worldwide.
In Australia, cardiovascular disease (CVD) affects around 1 in 17 Australian males and becomes more common as you get older. It causes more than one in four deaths.
How much you move, and the food and drink you consume, play a big part in helping reduce your CVD risk, and your cholesterol levels also play a role.
Most people know cholesterol is important in some way, but what exactly is it, how does it affect you and what should you do about it?
Let’s investigate.
What is cholesterol?
Cholesterol is a fatty molecule that is needed for our bodies to function. It is made by our liver or comes from our diet, and is transported in our blood in particles called low-density lipoprotein (LDL) or high-density lipoprotein (HDL).
LDL transports cholesterol to the cells and tissues of the body, whereas HDL carries cholesterol from the tissue to the liver.
Often, LDL is called ‘bad cholesterol’ and HDL is called ‘good cholesterol’.
Various factors affect blood cholesterol levels including your diet and lifestyle, body weight and genes.
Why is high cholesterol bad for you?
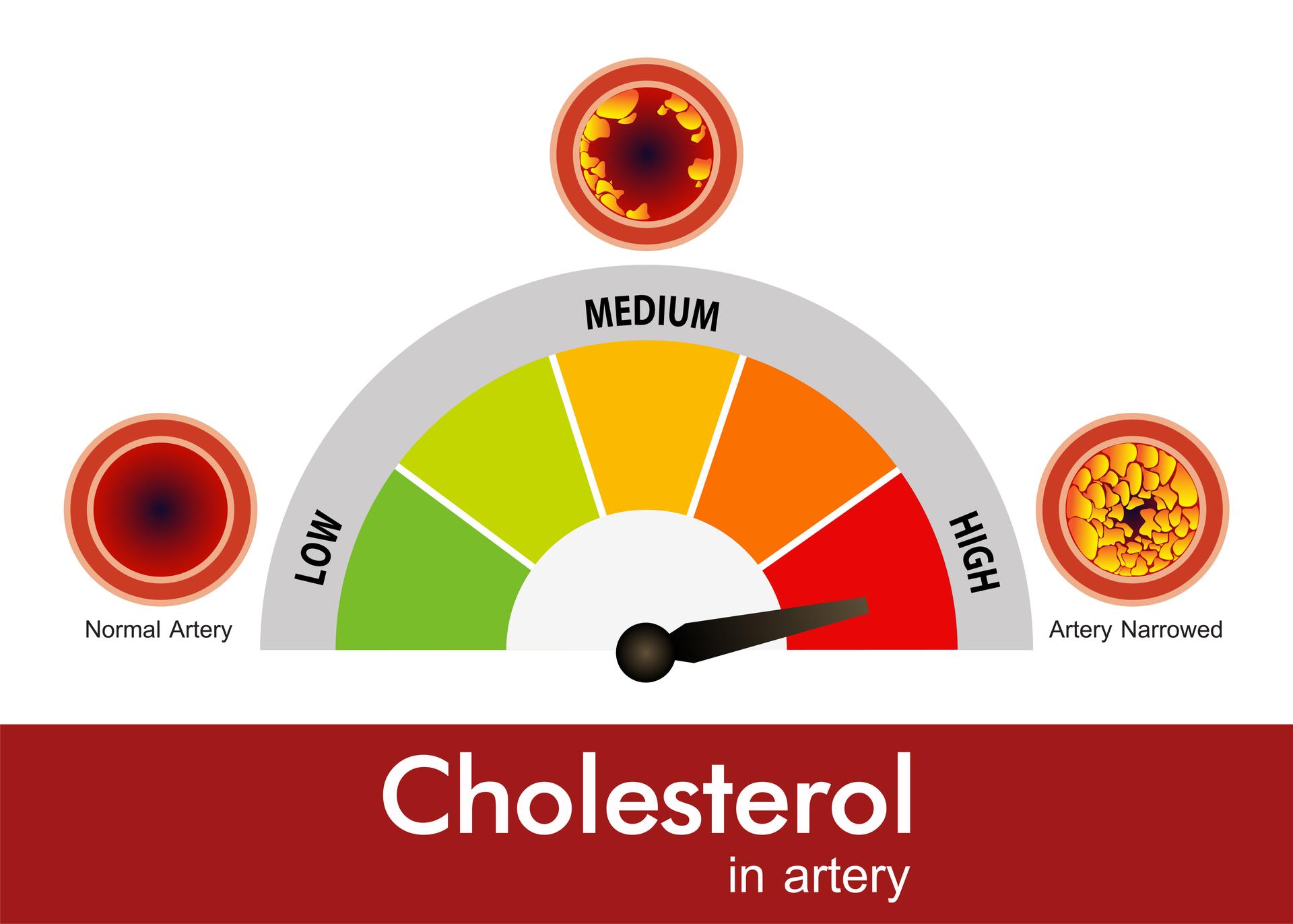
If you have too much LDL in your blood, you can develop fatty deposits in your blood vessels which makes it harder for blood to flow through the arteries.
If the deposits break apart, they can form a blockage that leads to a heart attack or stroke.
How is cholesterol tested?
Cholesterol is measured with a blood test called a lipid panel or lipid profile.
The test measures total cholesterol, HDL and LDL, as well as triglycerides, which are another type of fat in the blood.
Usually, you’ll be asked to fast (not eat anything) and only drink water for about 10 hours before the test.
If your LDL levels are high, your doctor will recommend lifestyle changes to reduce your levels or prescribe medication (or both).
What are the signs and symptoms of high cholesterol?
According to the Heart Foundation, high cholesterol generally doesn’t have obvious symptoms, which is why it’s important to get a blood test and regular check-ups.
If you are 45 or older (35 or older, if you are Aboriginal or Torres Strait Islander), see your doctor for a cholesterol test.
If you have a family history of high cholesterol, speak to your GP about your heart disease risk.
Lifestyle changes that can help
There are some easy lifestyle changes you can make to reduce your ‘bad’ cholesterol. Heart disease takes years to develop, so taking steps to reduce your levels now will be beneficial now and in the future.
Why high cholesterol is particularly problematic for the Aboriginal and Torres Strait Islander community
Unfortunately, CVD is even more of an issue for Aboriginal and Torres Strait Islander people than it is for non-Indigenous individuals.
It is the largest contributor to the health gap between Indigenous and non-Indigenous Australians, is the leading cause of death among Aboriginal and Torres Strait Islander people, and affects them at relatively younger ages.
According to Australian Indigenous HealthInfoNet, this is partly because the “risk factors for cardiovascular disease are common among (Aboriginal and Torres Strait Islander) people.
Many of the cardiovascular diseases share risk factors such as tobacco smoking, physical inactivity, being overweight and obese, diabetes and high cholesterol.”
Because of this, Aboriginal and Torres Strait Islander people should have their cholesterol levels checked earlier than non-Indigenous Australians; it’s recommended Aboriginal and Torres Strait Islander individuals be tested every five years starting from the age of 35, which is 10 years earlier than non-Indigenous people.