Vasectomy is a safe and reliable means of permanent contraception that’s growing in popularity among younger Australian males (see Figure).
Some health professionals are reluctant to recommend vasectomy for young men because of its irreversible effect on fertility and the possibility that — with changes to personal circumstances over time — they may change their minds. Vasectomy reversal or testicular sperm extraction might be possible for some men to father children after a vasectomy, but these procedures are not always successful and have significant costs.
Although there are no absolute contraindications to vasectomy[1] a man’s age, and whether he has children, are important to consider when counselling anyone about the procedure.
General practice is a common setting for discussions about contraception; albeit far more common for female patients than males[2].
Limitations in health practitioners’ knowledge about vasectomy may contribute to underutilisation of the procedure, thereby concentrating responsibility for couples’ contraception on females[3]. This is demonstrated by higher rates of tubal ligation in women than vasectomy in males, even though vasectomy is a simpler, shorter and safer operation.
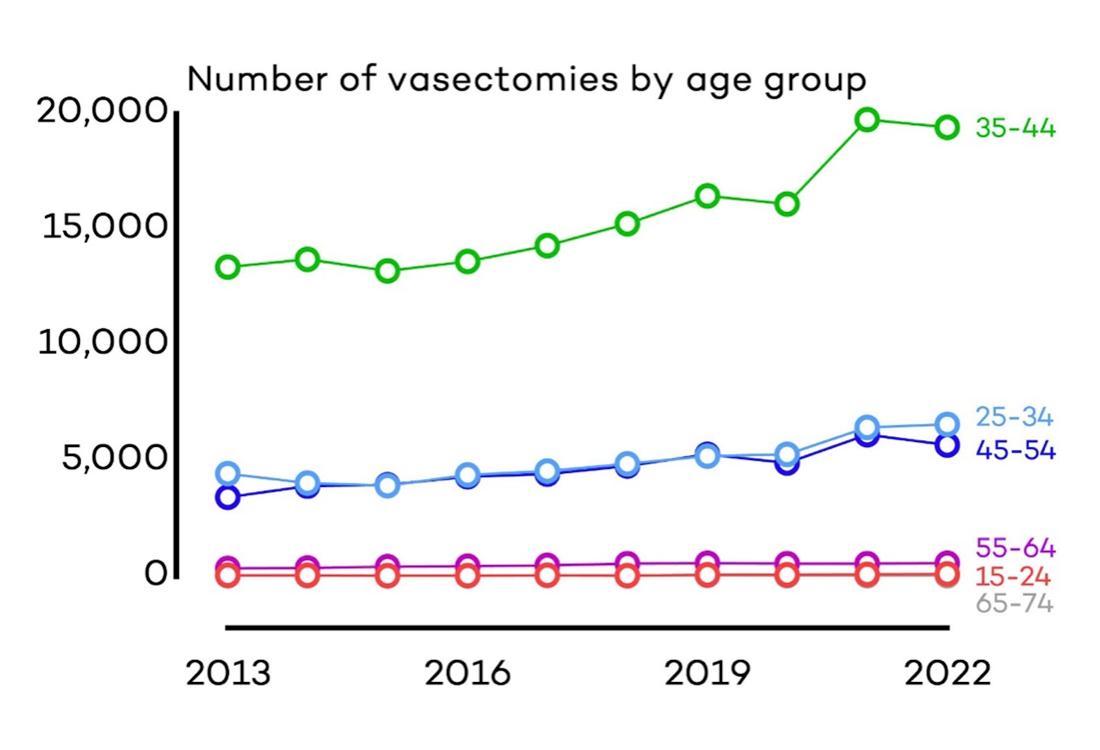
Fig 1 – Number of vasectomies by age group since 2013
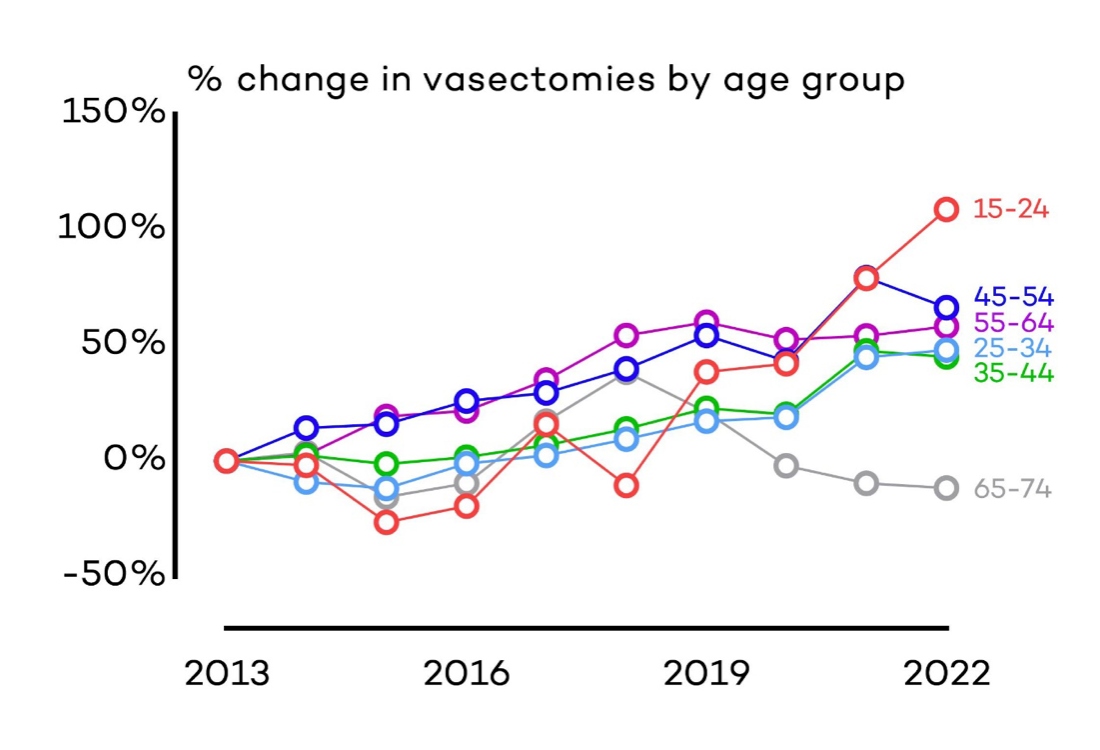
Fig 2 – Percentage change in vasectomies by age group since 2013
None of the items in the list above apply any more or less to young men than older men.
A recent US study found that among men who were childless at the time of their vasectomies, which were conducted between 2004 and 2017, none sought reversal during the intervening period (up to 14 years)[6].
The researchers suggest that men without children who seek vasectomy are subjected to greater scrutiny than fathers, reflecting bias on the part of the providers (likely fostered by our society’s value of procreation). The study’s senior author recognises that having a vasectomy “is an incredibly personal decision for every patient”, and “it’s not our place to ask social questions and steer [men without children] away from the procedure”.
A young man’s decision to have a vasectomy is his to make. The role of health providers is to ensure he is counselled in the same way as any other man.
References
[1] Dohle et al., 2012. European Association of Urology Guidelines on Vasectomy. European Urology.
[2] Velez, et al., 2021. Vasectomy: a guideline-based approach to male surgical contraception. Fertility & Sterility.
[3] Tcherdukian et al., 2022. Knowledge, professional attitudes, and training among health professionals regarding male contraceptive methods. The European Journal of Contraception & Reproductive Health Care.
[4] Harris & Holmes, 2001. Requests for Vasectomy: Counselling and Consent. Journal of the Royal Society of Medicine
[5] Sharlip et al., 2012. Vasectomy: AUA Guideline. Journal of Urology
[6] Bryk et al., 2020. Childless men at the time of vasectomy are unlikely to seek fertility restoration. Urology