Background
In 2017, over 16,500 Australian men were estimated to receive a diagnosis of prostate cancer, making this the most commonly diagnosed cancer in men over 50.
Localised prostate cancer is treated in several ways, including: active surveillance, open or robotic prostatectomy (surgery), or radiotherapy. Large clinical studies have found no significant difference between treatment choice for localised prostate cancer and the rate of cure (1).
Both surgery and radiotherapy treatments can negatively impact quality of life scores but the specific side-effects vary; urinary incontinence and erectile dysfunction is more likely with surgery, and bowel dysfunction is more likely with radiotherapy (2).
While shared treatment decision-making is advocated, there is no singular pathway that Australian men with low-risk prostate cancer or their doctors are required to take.
A small research study carried out by an impartial research team at a public hospital in NSW examined the decision making process for men with localised prostate cancer, where robotic surgery or radiotherapy would be equally appropriate treatment options.
Aim
The Prostatectomy versus Radiotherapy for Early-stage PRostatE cancer (PREPaRE) study aimed to understand how men treated at the Liverpool Hospital (Sydney) come to decisions about their prostate cancer treatment, and the best ways to support men in choosing a treatment that most suits them.
Methods
The qualitative study was conducted in 2017 at Liverpool Hospital. Patients diagnosed with localised prostate cancer underwent a combined clinic, meeting with a urologist and a radiation oncologist, to facilitate informed decision making around their treatment plan.
The information provided to the patient was guided by the clinician delivering the consultation. Patients who participated in the study (n=25) had localised prostate cancer and were suitable for either radiotherapy or robotic surgery treatments.
Patients had appointments with a urologist at least twice (for biopsy and diagnosis) before attending the combined clinic.
The study participants completed surveys and interviews before and/or after the combined clinic appointment to assess: the men’s understanding of the robotic prostatectomy and radiotherapy treatments; what their preferences were and their reasons for selecting a specific treatment; and what information and decision aids they found helpful.
Results
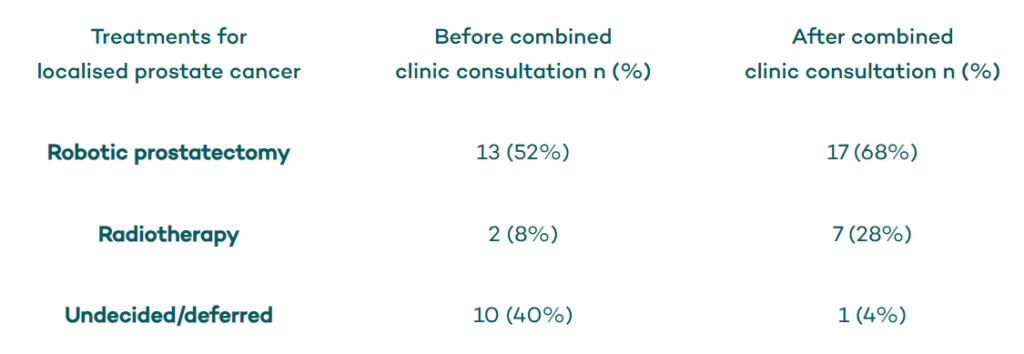
Men’s initial treatment preferences and subsequent treatment decisions after the combined clinic are shown in the Table.
Major Themes (See Subthemes in Notes)
Conclusions
The authors conclude that men with localised prostate cancer should see both a urologist and a radiation oncologist to make a fully informed decision about their treatment, and that this should be done earlier in the patient’s care (i.e. at diagnosis).
The authors recommended more education to improve patients’ understanding about the difference between radical prostatectomy and radiotherapy and about their specific side effects.
Tailored strategies to best support and inform men about treatments for prostate cancer are needed.














